Tooth extraction is a common dental procedure that involves removing a tooth due to decay, trauma, crowding, or other complications.
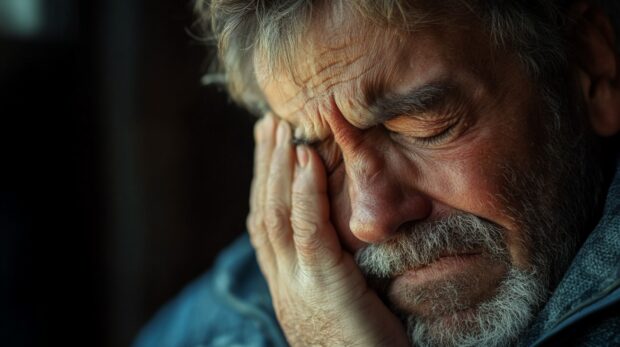
Recovery generally progresses over several days. Pain and swelling typically decrease after the first 72 hours, and most patients notice significant improvement by day 7.
Persistent or worsening pain after a week may indicate complications that require professional attention. It’s important to monitor symptoms closely and seek help if discomfort escalates instead of improving.
We’ve decided to talk with people from TannlegeTeam and learn what people can expect 7 days after tooth extraction.
What’s Normal at Day 7?
By the seventh day after a tooth extraction, mild discomfort may still be present, especially in cases involving wisdom teeth or surgical extractions.
Most individuals notice a gradual improvement compared to the first few days post-surgery.
Some lingering tenderness near the extraction site is expected. Swelling may still be visible but should be subsiding.
The body’s natural healing process results in the formation of scabbing or granulation tissue, a soft layer that begins to cover and protect the socket.
- Slight sensitivity near the site
- Decreasing swelling
- Gradual restoration of normal eating and talking
- Absence of new or sharp pain
Feeling noticeably better than earlier in the week generally points toward proper healing.
Any deviation from steady improvement should be noted and brought to a dental provider’s attention.
Prioritize your health and make the right choices at the right time.
When Pain Isn’t Normal: Warning Signs
Pain that intensifies instead of lessening after a week can signal trouble. Sudden spikes in discomfort, especially sharp or radiating pain, should never be ignored.
Radiating pain that spreads to the ear, neck, jaw, or eye area may indicate nerve involvement or infection.
Additional red flags include a foul odor or taste coming from the socket, which could suggest dry socket or bacterial activity.
Visible pus, persistent swelling, or fever are also signs of a possible infection. Bone that becomes exposed or visible in the extraction site is never a normal part of healing and requires urgent evaluation.
- Sharp, worsening pain
- Pain radiating to other facial areas
- Bad breath or unpleasant taste
- Fever or increased swelling
- Visible bone or pus
Prompt dental consultation is crucial to avoid worsening the issue or developing systemic infection.
Common Causes of Pain After 7 Days
Pain lingering beyond the expected recovery window of a tooth extraction is often a sign that something isn’t progressing as it should.
Most individuals begin to feel better by day seven, so any new or worsening discomfort at that point can be linked to underlying complications.
Multiple conditions can interfere with healing, each with its own set of symptoms and risk factors.
Identifying the cause of pain is the first step in receiving effective treatment and avoiding further dental or systemic issues.
Dry Socket (Alveolar Osteitis)
Dry socket remains one of the most painful complications following tooth extraction.
It occurs when the protective blood clot either dissolves prematurely or is dislodged, exposing underlying bone and nerve endings to air, food, and fluids.
- Intense throbbing pain that often begins around day 3–5
- Foul taste or odor
- Bone is visible in the socket
Common triggers include smoking, vigorous rinsing, drinking through a straw, or poor oral hygiene.
Preventive care involves gentle cleaning and adherence to the dentist’s aftercare instructions. Immediate treatment typically includes medicated dressings and pain relief.
Infection at the Extraction Site
Bacterial infection can disrupt the healing process and spread if not addressed promptly.
Infection often develops after bacteria infiltrate the socket, especially in individuals with compromised immune systems or poor oral care routines.
- Persistent or worsening pain
- Throbbing sensation
- Fever, pus, or excessive swelling
- Swollen lymph nodes

People with diabetes or those undergoing treatments that lower immunity face increased risk.
Dentists usually respond by prescribing antibiotics and performing a thorough cleaning of the affected area.
Residual Tooth or Bone Fragments
Occasionally, fragments of bone or tooth remain in the socket after extraction.
While small pieces might surface and come out on their own, others may stay lodged in the tissue and trigger irritation or inflammation.
- A poking or sharp sensation at the site
- Localized swelling or discomfort that doesn’t fade
- Difficulty chewing or brushing near the area
Dental professionals can perform a minor procedure to remove debris and allow proper healing. Leaving fragments untreated may delay recovery and cause ongoing irritation.
Nerve Damage
Nerve-related pain typically occurs after extractions involving the lower jaw, particularly wisdom teeth.
Nerve damage isn’t always permanent, but it may last for weeks or months depending on the severity.
- Numbness in the lip, chin, or tongue
- Tingling or electric-shock-like sensations
- Changes in taste perception
- Prolonged or shooting pain

Dentists and oral surgeons monitor nerve-related symptoms carefully.
Persistent or worsening sensory changes should be assessed with advanced imaging and possibly referred to a specialist for evaluation.
Sinus Complications (Upper Teeth Only)
Upper molars and premolars are positioned near the sinus cavities.
In some cases, extraction may accidentally create a communication between the mouth and sinus, known as a sinus perforation.
- Nasal discharge or drainage through the socket
- Pressure in the cheeks or forehead
- Pain that worsens with nose-blowing or bending forward
Dentists can test for sinus involvement and treat minor cases with antibiotics and nasal precautions. Larger perforations may require intervention by an ENT specialist.
Adjacent Tooth Irritation
Nearby teeth sometimes become irritated during or after an extraction.
Referred pain or inflammation can cause discomfort that seems unrelated to the actual extraction site.
- Mimic the feeling of a cavity or fracture
- Seem like it originates from a different tooth
- Intensify during chewing or brushing

Inflammation usually fades as the area heals. If pain persists, dentists may take x-rays to rule out other dental problems or lingering trauma.
Delayed Healing
Healing may be slower than expected due to health conditions or lifestyle choices. Smoking restricts blood flow, which impairs healing.
Nutritional deficiencies, dehydration, and chronic illnesses such as diabetes also play a role.
- Prolonged tenderness or pain
- Unusual tissue appearance around the socket
- Fatigue or sluggish recovery process
People dealing with systemic health issues or taking medications that affect circulation should follow up closely with their dental provider.
Proper intervention can redirect the healing process and prevent complications from becoming severe.
What to Do If You’re in Pain After 7 Days
Persistent pain after a week is not something to ignore. Contacting your dentist promptly ensures that emerging issues don’t escalate.
Dentists will examine the site, possibly take x-rays, and clean the socket if needed. Depending on the cause, treatment might include pain relief, antibiotics, or surgical removal of debris.
- Physical examination of the socket
- Imaging to detect infection, fragments, or sinus involvement
- Cleaning or dressing the site
- Prescriptions for medication if needed
Acting quickly helps minimize complications and promotes faster healing.

Treatment Options
Pain can often be managed with over-the-counter medication such as ibuprofen or acetaminophen.
Cold compresses help reduce swelling and numb the area.
For dry socket, dentists may apply medicated dressings to protect the bone and reduce discomfort.
Antibiotics are prescribed for confirmed infections, and lingering fragments may be surgically removed.
- Pain relief: ibuprofen, acetaminophen, cold packs
- Dry socket care: socket rinsing, medicated dressing
- Infection control: antibiotics and possible drainage
- Fragment removal: minor surgery if needed
Following aftercare instructions and maintaining good hygiene are critical to effective recovery.
Summary
Mild discomfort a week after extraction can be normal, especially for difficult procedures. Intense or worsening pain, however, is a sign that something might be wrong.
Recognizing symptoms early and seeking help makes a major difference in recovery. Dental professionals can identify problems quickly and provide effective treatment.
When in doubt, scheduling a follow-up visit is always the safest choice. Let your mouth heal properly—don’t wait for pain to force action.
 Jewel Beat
Jewel Beat

